Why is the Delta variant such a worry?
The Delta variant is driving waves of COVID-19 infections all around the world
July 06, 2021
While Australians may be focused on the havoc the Delta variant is wreaking on our shores, Delta is in fact driving waves of COVID infections all around the world.
With the World Health Organisation (WHO) warning Delta will rapidly become the dominant strain, let’s take a look at this variant in a global context.
The Delta variant (B.1.617.2) emerged quietly in the Indian state of Maharashtra in October 2020. It barely caused a ripple at a time when India was reporting around 40,000 to 80,000 cases a day, most being the Alpha variant (B.1.1.7) first found in the United Kingdom.
That changed in April when India experienced a massive wave of infections peaking at close to 400,000 daily cases in mid-May. The Delta variant rapidly emerged as the dominant strain in India.
The WHO designated Delta as a variant of concern on May 11, making it the fourth such variant.
The Delta variant rapidly spread around the world and has been identified in at least 98 countries to date. It’s now the dominant strain in countries as diverse as the UK, Russia, Indonesia, Vietnam, Australia and Fiji. And it’s on the rise.
In the United States, Delta made up one in five COVID cases in the two weeks up to June 19, compared to just 2.8% in the two weeks up to May 22.
Meanwhile, the most recent Public Health England weekly update reported an increase of 35,204 Delta cases since the previous week. More than 90% of sequenced cases were the Delta variant.
In just two months, Delta has replaced Alpha as the dominant strain of SARS-CoV-2 in the UK. The increase is primarily in younger age groups, a large proportion of whom are unvaccinated.
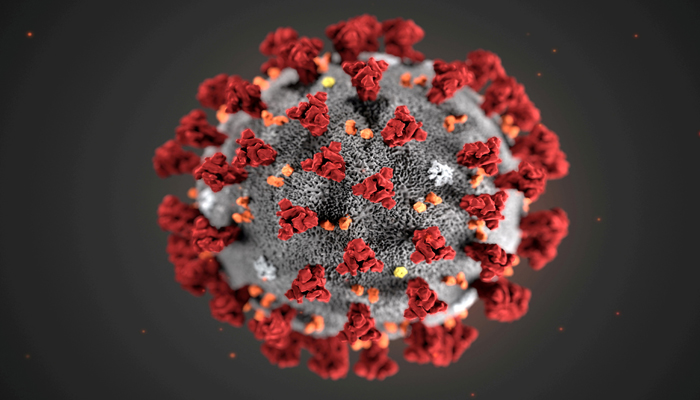
Scientists have identified more than 20 mutations in the Delta variant, but two may be crucial in helping it transmit more effectively than earlier strains. This is why early reports from India called it a “double mutant”.
The first is the L452R mutation, which is also found in the Epsilon variant, designated by the WHO as a variant of interest. This mutation increases the spike protein’s ability to bind to human cells, thereby increasing its infectiousness.
Preliminary studies also suggest this mutation may aid the virus in evading the neutralising antibodies produced by both vaccines and previous infection.
The second is a novel T478K mutation. This mutation is located in the region of the SARS-CoV-2 spike protein which interacts with the human ACE2 receptor, which facilitates viral entry into lung cells.
The recently described Delta Plus variant carries the K417N mutation too. This mutation is also found in the Beta variant, against which COVID vaccines may be less effective.
One good thing about the Delta variant is the fact researchers can rapidly track it because its genome contains a marker the previously dominant Alpha variant lacks.
This marker — known as the “S gene target” — can be seen in the results of PCR tests used to detect COVID-19. So researchers can use positive S-target hits as a proxy to quickly map the spread of Delta, without needing to sequence samples fully.
The most feared consequences of any variant of concern relate to infectiousness, severity of disease, and immunity conferred by previous infection and vaccines.
WHO estimates Delta is 55% more transmissible than the Alpha variant, which was itself around 50% more transmissible than the original Wuhan virus.
That translates to Delta’s effective reproductive rate (the number of people on average a person with the virus will infect, in the absence of controls such as vaccination) being five or higher. This compares to two to three for the original strain.
There has been some speculation the Delta variant reduces the so-called “serial interval”; the period of time between an index case being infected and their household contacts testing positive. However, in a pre-print study (a study which hasn’t yet been peer-reviewed), researchers in Singapore found the serial interval of household transmission was no shorter for Delta than for previous strains.
One study from Scotland, where the Delta variant is predominating, found Delta cases led to 85% higher hospital admissions than other strains. Most of these cases, however, were unvaccinated.
The same study found two doses of Pfizer offered 92% protection against symptomatic infection for Alpha and 79% for Delta. Protection from the AstraZeneca vaccine was substantial but reduced: 73% for Alpha versus 60% for Delta.
A study by Public Health England found a single dose of either vaccine was only 33% effective against symptomatic disease compared to 50% against the Alpha variant. So having a second dose is extremely important.
In a pre-print article, Moderna revealed their mRNA vaccine protected against Delta infection, although the antibody response was reduced compared to the original strain. This may affect how long immunity lasts.
The Delta variant is more transmissible, probably causes more severe disease, and current vaccines don’t work as well against it.
WHO warns low-income countries are most vulnerable to Delta as their vaccination rates are so low. New cases in Africa increased by 33% over the week to June 29, with COVID-19 deaths jumping 42%.
There has never been a time when accelerating the vaccine rollout across the world has been as urgent as it is now.
WHO chief Tedros Adhanom Gebreyesus has warned that in addition to vaccination, public health measures such as strong surveillance, isolation and clinical care remain key. Further, tackling the Delta variant will require continued mask use, physical distancing and keeping indoor areas well ventilated.











