COVID-19: A virulent spectre that continues to stalk the survivors
While many finally recuperated, others were left struggling with a perturbing question: Will they ever feel normal again?

Nearly five years have passed since the world was locked down to stop the spread of COVID-19 — a virus that infected over 778 million people and took 7.1 million lives globally. While many finally recuperated, others were left struggling with a perturbing question: Will I ever feel normal again?
It's been almost five years from the time when the world went into a lockdown owing to COVID-19, which has since infected 778m people globally and claimed 7.1 million lives. As the world moved forward, many COVID-19 patients came to terms with the fear that they may never fully recover.
COVID-19 has shown the potential to cause long-term health complications, commonly referred to as post-COVID-19 condition (PCC) or Long COVID. These symptoms typically arise within three months of the initial infection and persist for at least two months — often much longer. According to the World Health Organization (WHO), about 6 in every 100 people who contract COVID-19 develop post-COVID conditions. These estimates are mostly based on early-pandemic data. More recent figures from 2022 suggest that up to 15 in every 100 people still report symptoms even a year after infection.
Long COVID encompasses a range of symptoms; common manifestations include fatigue, cognitive impairments ("brain fog"), shortness of breath, and chest pain. The condition affects individuals across all age groups and health backgrounds, including those who experienced mild or asymptomatic initial infections. Global estimates suggest that approximately 65 million people have Long COVID.
A 2023 study conducted in Pakistan surveyed 300 participants. Among them, 155 had tested positive for COVID-19, and 54 reported symptoms lasting more than 12 weeks — meeting the criteria for Long COVID. Muscle pain and fatigue were the most frequently reported symptoms (14.7%), followed by breathing difficulties and cognitive issues (both 12.6%).
Participants who had experienced loss of appetite or confusion during their acute illness were more likely to develop Long COVID. The majority of respondents (83.3%) reported moderate levels of stress, while 17.3% suffered moderate to severe stress.
Seventy-year-old Muhammad Aslam Shah contracted COVID-19 two years ago. A history of smoking worsened the infection’s impact on his lungs, causing irreversible shrinkage. He underwent an extended booster vaccination course and, although he began to recover after five to six months, he still depends on medication and sometimes requires a nebuliser.
In winter, especially, he experiences chest congestion or a throat infection and faces more breathing difficulties, so doctors recommend booster shots for him, and he has to go for routine checkups.
Importantly, Long COVID doesn’t depend on how sick someone was during their initial infection.

Masooma Bashir, 26, caught COVID-19 during the first wave and recovered within a month — or so she thought. Later, she began experiencing persistent symptoms: joint pain, extreme hair loss, digestive issues, and hypersensitivity.
“The worst part was the shortness of breath — dyspnea — something I had never felt before COVID,” she recalled.
Even years later, she still feels its effects. She also developed an eye infection that her doctor linked to COVID-19.
Her father, Muhammad Bashir Khadim, 70, was infected around the same time. His condition was critical — he spent 22 days at Mayo Hospital and another month at Sheikh Zayed Hospital.
His recovery took more than two months, but the aftermath lingered.
“He developed a severe ear infection that lasted six months,” Masooma said.
“When we saw a doctor, they told us it was a post-COVID infection and would take time to heal.” Bashir also lost his sense of taste and smell for an extended period and still suffers from joint pain.
Dr Muhammad Taimoor, a pulmonologist with over 40 years of experience, told Geo.tv that Long COVID is still common in Pakistan.
“Even now, patients come in saying they lost their sense of taste or smell after COVID — and it hasn’t returned,” he said.
Families also report mental disorientation, and post-COVID lung scarring (fibrosis) is frequently observed. Some of these conditions, like fibrosis, are permanent, while others vary in duration and can be treated.
Not everyone seeks medical attention, but they still experience lingering symptoms.
Farhan Nasir, 30, said he’s been dealing with joint pain, hypersensitivity, and breathing issues since recovering from COVID-19.
Ahmed Aslam, 25, described a decline in his overall stamina. “Before COVID, I could work five hours straight. Now, after two or three hours, I’m drained — mentally and physically. Maybe age plays a part, but this started after COVID.”
Many Long COVID patients initially have mild infections, avoid hospitalisation, and only come to recognise an issue later when their symptoms persist. While some fully recover, others notice gradual improvements over time.

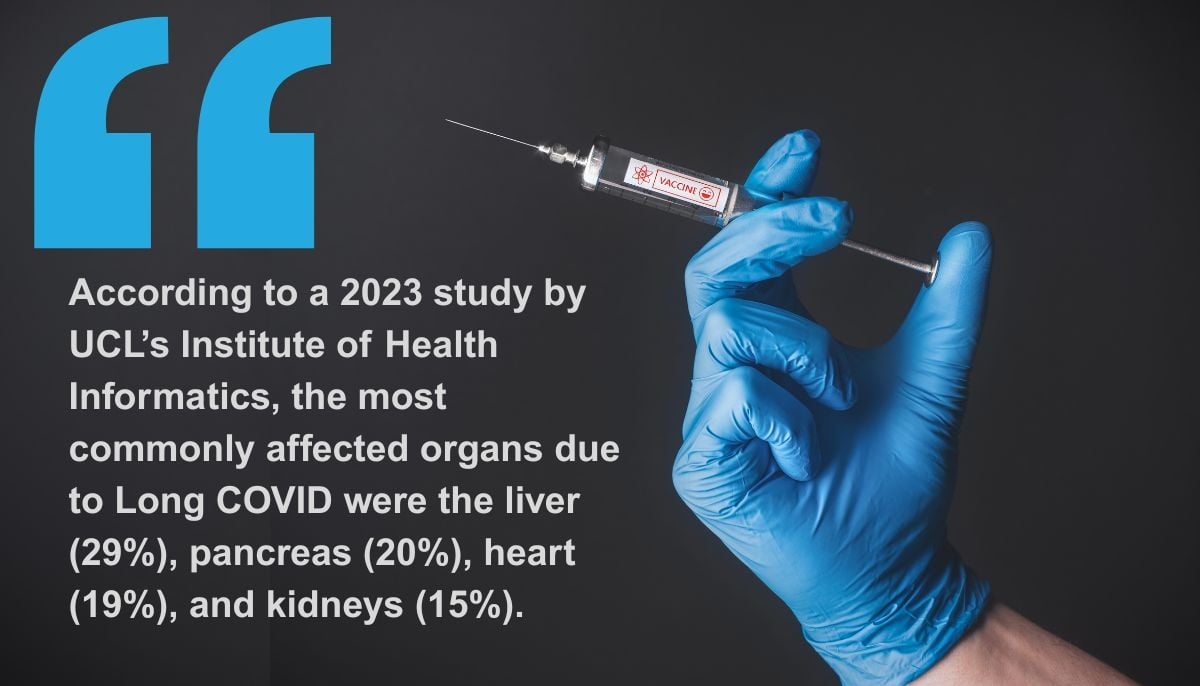
A 2023 study led by Professor Amitava Banerjee at the University College London's Institute of Health Informatics followed 536 Long COVID patients. Using MRI scans, the researchers assessed heart, lung, liver, kidney, and pancreas damage six months after infection.
Remarkably, only 13% of the patients had been hospitalised, and just 2% had received at least one vaccine dose.
Their initial scans revealed that 62% of the participants (331 individuals) showed signs of organ damage. The most commonly affected organs were the liver (29%), pancreas (20%), heart (19%), and kidneys (15%). These 331 participants were re-evaluated six months later through a follow-up MRI scan.
After one year, they observed that 59% of the original participants still had impairment in at least one organ, while 27% experienced impairment in two or more organs.
This indicates that for the majority of participants with organ damage at six months, the impairment persisted for at least 12 months.

Dr Muhammad Ahmed, a pulmonologist with 13 years of experience, said Long COVID symptoms often persist long after recovery.
“It’s not just COVID — we’ve seen this after pneumonia, TB, or even cancer,” he explained.
Patients who were critically ill or required oxygen or high-dose medications are more likely to experience lasting damage.
Dr Ahmed listed fatigue, headaches, persistent cough, reduced stamina, low mood, depression, and loss of taste or smell as the most common post-COVID complaints.
Who is most at risk — and why do some people bounce back while others don’t? Dr Ahmed pointed to existing health conditions.
“Age is a major factor, along with diabetes and other chronic illnesses. But we’ve also seen young people — especially those living alone — develop Long COVID.”
Some studies suggest that in certain patients, the immune system goes into overdrive, flooding the body with immune cells and triggering chronic inflammation.
Dr Laura Bergamaschi, lead author of one such study, explained: "Some immune cells continue to behave abnormally even after recovery. Some regenerate slowly, while others, like certain T and B cells, remain overly active."
Dr Ahmed said there’s no definitive link between overall immunity and Long COVID, but patients sometimes report that their immunity improved after infection or vaccination. “Still, we’ve noticed new respiratory issues — like allergic rhinitis, asthma, or persistent flu — appearing in people who never had such conditions before.”
A 2024 study titled Exploring Neurocognitive and Emotional Outcomes of Long COVID on Pakistani Patients highlighted serious mental health effects, especially among women.
The study urged health officials to offer gender-sensitive mental health care as part of post-COVID recovery plans.
It also noted that patients with ADHD who experienced severe COVID-19 symptoms faced greater cognitive decline, heightened anxiety, depression, and even feelings of punishment.
However, recovery is possible.
Dr Ahmed emphasised that many patients improve through small lifestyle changes — daily walks, multivitamins, magnesium supplements, and emotional support from family. “Those who stay active and socially connected tend to recover faster,” he said.
COVID-19 reinfections are possible, and each carries the risk of Long COVID. According to the WHO, preventive measures like mask-wearing, hand hygiene, and ventilation remain important.
Long COVID continues to impact people of all ages and backgrounds. While some have healed, many still struggle with fatigue, breathing problems, and emotional stress. Experts agree: a holistic approach — combining medication, exercise, good nutrition, and strong social support — offers the best chance at recovery. But for those with lasting complications, long-term medical care is essential to regain a decent quality of life.
Momna Tahir is a staffer at Geo News.
Header and thumbnail illustration by Geo.tv